Posted by: Clear Advantage in Featured, Uncategorized on October 26, 2022
Did you know that all eyes are not always perfectly round? Some people’s eyes can start to bulge, changing their shape. When you have keratoconus, it causes the shape of the eyes to become irregular and affects your ability to see.
One in every 2,000 people has keratoconus. It develops gradually, usually beginning in adolescence and progressing until your mid-thirties.
Keratoconus affects the shape of your cornea. The cornea is the transparent part found at the front of your eye. When the shape of the cornea changes, it leads to adverse changes in vision.
There is no known way to prevent keratoconus, but there are ways to treat it and stop it from getting worse. Keep reading to learn more about keratoconus and how to treat it!
What is Keratoconus?
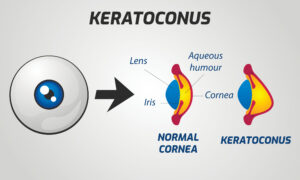
Also referred to as “KC,” keratoconus is an eye condition that causes the cornea to thin and begin bulging out from the eye. A healthy cornea is round and shaped like a dome.
When you have keratoconus, the cornea becomes more cone-shaped. Keratoconus is a progressive eye condition. It usually worsens over one to two decades.
It typically affects both eyes but can affect them differently. Keratoconus progresses gradually.
If you have this eye condition, you may not notice it at first. Most patients begin to see changes to their vision during adolescence.
Without treatment, it continues to worsen until a person reaches their mid-thirties. Eventually, your vision can become seriously impaired.
In the early stages of keratoconus, you can experience blurry or distorted vision. There may be a continuous static or snow-like effect on your sight. Little flickering dots can appear everywhere you look.
You may also have increased sensitivity to bright lights. As a result, glare and halos can be common, making it incredibly difficult to see at night.
With keratoconus, your vision may suddenly worsen or become clouded. You may also need frequent prescription changes.
What Causes Keratoconus?
The exact cause of keratoconus is unknown. In patients with keratoconus, collagen is often lost in the cornea.

Collagen is an essential structural component that allows your eye to keep its shape. You may lose collagen if the cells of the cornea cannot produce enough corneal tissue.
Some known factors can increase your risk of developing keratoconus. One of the most significant factors is age because it’s often diagnosed during adolescence for patients with keratoconus.
Your genetics may also play a role. Your chances of developing keratoconus may increase if you have a family history of keratoconus or other disorders.
These may include Downs syndrome and asthma. In patients with keratoconus, 10% have a parent with the disease.
Also affecting your chances of developing keratoconus are eye inflammation and rubbing. When your eyes are irritated, it can lead to destroying tissues in the cornea and causes severe damage to your eyes.
Chronically rubbing your eyes has been linked with keratoconus as well. It may cause the condition to worsen.
How is Keratoconus Diagnosed and Treated?
Your eye doctor can diagnose keratoconus during an eye exam. During your eye exam, your ophthalmologist will review your medical and family history.
They can use several tests to help diagnose patients with this eye condition. They may take a computerized image that maps out the curvature of your cornea.

A slit-lamp exam can closely examine the cornea for abnormalities. A pachymetry test measures how thin your corneas are.
After receiving a keratoconus diagnosis, many eye doctors begin treatment with glasses or soft contact lenses. These can treat blurry vision.
However, patients with keratoconus may notice that they need frequent prescription changes to continue improving their vision. These frequent visual changes are due to the cornea’s continuous change in shape.
The next recommendation for keratoconus patients is typically rigid contact lenses. Rigid or hard contact lenses can hold their shape better than soft ones.

Patients can experience better vision when they wear rigid contact lenses than when they use soft contacts. You can have rigid contact lenses specially made to fit an irregular cornea.
Because they are rigid, these contact lenses can be uncomfortable. Many patients get used to them over time.
Others may have an intrastromal corneal ring segment (INTACS) implanted instead. INTACS are another option for vision improvement.
Glasses and contact lenses aim to improve a patient’s vision. However, although they can help you see better, they won’t stop the progression of keratoconus.
What is Corneal Cross-Linking?
To stop the progression of keratoconus, your eye doctor may recommend corneal cross-linking. Corneal cross-linking is one of the only ways to prevent keratoconus from worsening.
Corneal cross-linking creates new bonds between the collagen fibers in your cornea, which helps to strengthen them. The procedure uses ultraviolet (UV) light and riboflavin (vitamin B2) eye drops.
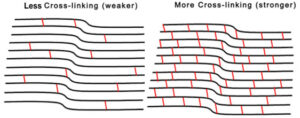
Keratoconus weakens your corneas. The new bonds created during corneal cross-linking help to restrengthen your cornea, allowing it to retain its shape.
Corneal cross-linking is the only FDA-approved treatment for progressive keratoconus and corneal ectasia. It allows you to avoid the need for a corneal transplant in the future.
In use for almost two decades, this outpatient procedure only takes about two hours to complete. You can go home to rest and recover after it’s over.
Most patients can return to their normal activities within a day or two. Plus, since it is considered “medically necessary,” it is covered by insurance.
Are you experiencing any symptoms of keratoconus? Don’t let it get any worse. Schedule an appointment at Clear Advantage Vision Correction Center in Portsmouth, NH, today!
There’s no reason why your vision should keep you from seeing the world with crisp clarity! Aren’t you ready to love the way you see again?